Are there other names for base of thumb arthritis?
- 1st CMCJ (Carpo Meta-Carpal Joint) arthritis
- Trapezio-metacarpal joint arthritis
Relevant anatomy:
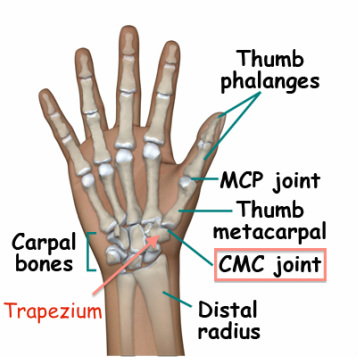
The thumb is formed of three bones. The distal phalanx has the nail attached to it, and is separated from the proximal phalanx by the Inter-Phalangeal Joint (IPJ). The proximal phalanx is connected to the 1st metacarpal bone by the MetaCarpo-Phalangeal Joint (MCPJ). Both the IPJ and MCPJ are simple hinge joints, essentially only allowing forward and backward movements (flexion and extension).
The thumb (or 1st) metacarpal bone sits on the trapezium, which is one of the eight wrist bones (carpal bones). This joint is called the 1st carpo meta-carpal joint (CMCJ) and is a multi-axial joint allowing movements in all directions, such that you can rotate your thumb in a circle. It is this large range of movements of this joint which is largely responsible for developing arthritis of your CMCJ.
The trapezium sits up against two other bones in your wrist, the scaphoid and trapezoid bones. Together these three bones form the Scapho-Trapezio-Trapezoid Joint (STT joint or STTJ). This joint can also be involved with arthritis, or rarely can be affected in isolation.
- 1st CMCJ (Carpo Meta-Carpal Joint) arthritis
- Trapezio-metacarpal joint arthritis
Relevant anatomy:
The thumb is formed of three bones. The distal phalanx has the nail attached to it, and is separated from the proximal phalanx by the Inter-Phalangeal Joint (IPJ). The proximal phalanx is connected to the 1st metacarpal bone by the MetaCarpo-Phalangeal Joint (MCPJ). Both the IPJ and MCPJ are simple hinge joints, essentially only allowing forward and backward movements (flexion and extension).
The thumb (or 1st) metacarpal bone sits on the trapezium, which is one of the eight wrist bones (carpal bones). This joint is called the 1st carpo meta-carpal joint (CMCJ) and is a multi-axial joint allowing movements in all directions, such that you can rotate your thumb in a circle. It is this large range of movements of this joint which is largely responsible for developing arthritis of your CMCJ.
The trapezium sits up against two other bones in your wrist, the scaphoid and trapezoid bones. Together these three bones form the Scapho-Trapezio-Trapezoid Joint (STT joint or STTJ). This joint can also be involved with arthritis, or rarely can be affected in isolation.

How does base of thumb arthritis develop?
Arthritis starts to develop as joint cartilage is worn away eventually exposing the underlying bone and causing pain when the joint moves. As well as pain, patients may notice a reduced range of motion of the thumb, stiffness, swelling and deformity around the base of the thumb. Base of thumb arthritis is normally a result of wear and tear over time, although can occasionally be associated with trauma, an abnormally shaped joint or inflammatory disease (e.g. rheumatoid arthritis). Hyperlaxity of joints, or hormonal changes resulting in increase ligament laxity around joints are also contributory factors. Cumulative trauma may hasten arthritis, however there is no good evidence that occupational overuse causes arthritis, rather that the symptoms are exposed due to the demands of work.
Arthritis starts to develop as joint cartilage is worn away eventually exposing the underlying bone and causing pain when the joint moves. As well as pain, patients may notice a reduced range of motion of the thumb, stiffness, swelling and deformity around the base of the thumb. Base of thumb arthritis is normally a result of wear and tear over time, although can occasionally be associated with trauma, an abnormally shaped joint or inflammatory disease (e.g. rheumatoid arthritis). Hyperlaxity of joints, or hormonal changes resulting in increase ligament laxity around joints are also contributory factors. Cumulative trauma may hasten arthritis, however there is no good evidence that occupational overuse causes arthritis, rather that the symptoms are exposed due to the demands of work.

How might base of thumb arthritis affect me?
To begin with there might only be an occasional ache at the end of a days work, with occasional sharper episodes when you “catch” your thumb in a certain way. Most people treat this by themselves by resting the thumb and taking simple analgesia. As things progress you may be continually troubled with pain, which can limit certain activities and eventually result in people avoiding using their hand altogether. Activities that require strength and/or mobility of the thumb are particularly difficult to perform, for instance:
- key pinch
- opening a jar
- writing
- playing instruments eg. piano, guitar or an instrument requiring a bow
- holding and manipulating certain tools
- sewing and crocheting by hand
- pain on shaking hands
What other diseases can cause pain in the same area?
There are many structures and other disease processes that occur around the base of the thumb which can also cause pain, and these include:
- STT arthritis
- De Quervain’s tenosynovitis
- Flexor carpii radialis tendonitis
- Carpal tunnel syndrome
- Trigger thumb
- Radio scaphoid arthritis
What are the treatment options for base of thumb arthritis?
1. Avoidance of those activities causing pain – easier said than done!
2. Pain killers (analgesics): starting with simple pain killers such as paracetamol and ibuprofen, and later adding in stronger pain killers such as codiene
3. Splinting the thumb – holds the thumb in positions that don’t cause pain
4. Steroid injection into the CMCJ
5. Denervation of the 1st CMCJ
6. Trapeziectomy (removal of the trapezium bone)
7. Trapeziectomy with tissue interposition (TI)
8. Trapeziectomy with ligament reconstruction and tissue interposition (LRTI)
Athough it seems quite a drastic step to take, removal of the trapezium bone is the only surgical solution shown to reliably treat base of thumb arthritis in the long term. Partial joint resections and joint replacements have not proven to be successful in treating 1st CMCJ arthritis.
Studies have found no difference between any of the forms of trapeziectomy. My standard operation is a trapeziectomy and tissue interposition (TI), which means placing some tissue in the space from where the trapezium bone is removed from. The technique I favour uses the joint capsule of the trapezium bone as the “tissue spacer” which would otherwise be left redundant, and does not involve any further cuts on the hand or arm. However if the thumb base is very unstable after removing the trapezium then I will perform a ligament reconstruction combined with a tissue interposition (LRTI) using one of the nearby tendons.
With increasing frequency I now perform a denervation procedure on the 1st CMCJ. This involves making a similar incision (cut) as with a trapeziectomy, but the trapezium is not removed. Instead the aim is to divide all the nerves to the trapezium, such that no pain is felt from the arthritis. However the results of this operation are variable, and may not completely remove the pain. When successful grip strength is not reduced, and may hopefully even increase, were as with trapeziectomy some loss of grip strength is expected.
What can I expect from the surgery?
Your hand will be bandaged, and a splint applied to your thumb to reduce movement and therefore pain. You will need to wear a splint for 6 weeks after surgery, and will require medium to strong pain killers during this period. After two weeks I will start to get you to move your thumb a bit. At six weeks I normally give you a soft splint for the thumb during the day, but keep the hard splint for night and heavier activities. It often takes between 6 and 12 months before all discomfort from the ope
To begin with there might only be an occasional ache at the end of a days work, with occasional sharper episodes when you “catch” your thumb in a certain way. Most people treat this by themselves by resting the thumb and taking simple analgesia. As things progress you may be continually troubled with pain, which can limit certain activities and eventually result in people avoiding using their hand altogether. Activities that require strength and/or mobility of the thumb are particularly difficult to perform, for instance:
- key pinch
- opening a jar
- writing
- playing instruments eg. piano, guitar or an instrument requiring a bow
- holding and manipulating certain tools
- sewing and crocheting by hand
- pain on shaking hands
What other diseases can cause pain in the same area?
There are many structures and other disease processes that occur around the base of the thumb which can also cause pain, and these include:
- STT arthritis
- De Quervain’s tenosynovitis
- Flexor carpii radialis tendonitis
- Carpal tunnel syndrome
- Trigger thumb
- Radio scaphoid arthritis
What are the treatment options for base of thumb arthritis?
1. Avoidance of those activities causing pain – easier said than done!
2. Pain killers (analgesics): starting with simple pain killers such as paracetamol and ibuprofen, and later adding in stronger pain killers such as codiene
3. Splinting the thumb – holds the thumb in positions that don’t cause pain
4. Steroid injection into the CMCJ
5. Denervation of the 1st CMCJ
6. Trapeziectomy (removal of the trapezium bone)
7. Trapeziectomy with tissue interposition (TI)
8. Trapeziectomy with ligament reconstruction and tissue interposition (LRTI)
Athough it seems quite a drastic step to take, removal of the trapezium bone is the only surgical solution shown to reliably treat base of thumb arthritis in the long term. Partial joint resections and joint replacements have not proven to be successful in treating 1st CMCJ arthritis.
Studies have found no difference between any of the forms of trapeziectomy. My standard operation is a trapeziectomy and tissue interposition (TI), which means placing some tissue in the space from where the trapezium bone is removed from. The technique I favour uses the joint capsule of the trapezium bone as the “tissue spacer” which would otherwise be left redundant, and does not involve any further cuts on the hand or arm. However if the thumb base is very unstable after removing the trapezium then I will perform a ligament reconstruction combined with a tissue interposition (LRTI) using one of the nearby tendons.
With increasing frequency I now perform a denervation procedure on the 1st CMCJ. This involves making a similar incision (cut) as with a trapeziectomy, but the trapezium is not removed. Instead the aim is to divide all the nerves to the trapezium, such that no pain is felt from the arthritis. However the results of this operation are variable, and may not completely remove the pain. When successful grip strength is not reduced, and may hopefully even increase, were as with trapeziectomy some loss of grip strength is expected.
What can I expect from the surgery?
Your hand will be bandaged, and a splint applied to your thumb to reduce movement and therefore pain. You will need to wear a splint for 6 weeks after surgery, and will require medium to strong pain killers during this period. After two weeks I will start to get you to move your thumb a bit. At six weeks I normally give you a soft splint for the thumb during the day, but keep the hard splint for night and heavier activities. It often takes between 6 and 12 months before all discomfort from the ope